Variants of GBS and CIDP
Dr. Karissa Gable from Duke University provided the following information about variants of GBS and CIDP, mimics, their symptoms, and how each are treated.
Understanding Variants
Unfortunately, there isn’t a single test that will determine whether someone has GBS, CIDP or MMN. Therefore, finding out if a patient has a variant or mimic is even harder to determine.
Doctors use a process of elimination to diagnose patients by using their symptoms, test results, and the progression of the patient’s illness and condition.
Variants differ from the typical symptoms because:
symptoms will affect some parts of the body more than others
some patients will come back with regular results in some tests while simultaneously having some tests with concerning data
variants take more time and more tests to determine
doctors must evaluate how a patient moves and what a patient can feel separately in order to understand if there are variants present as some variants can solely affect motor nerves or sensory nerves.
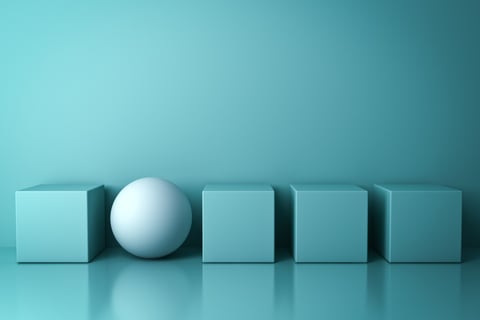
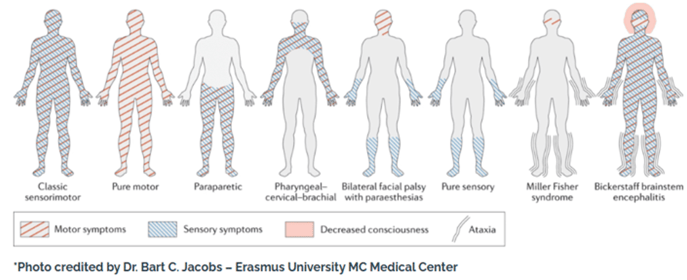
GBS Variants
Pharyngeal-cervical-branchial variant affects both motor and sensory muscles in the face and, in some cases, the arms as well.
Bilateral facial palsy cases include weakness in the face and only sensory symptoms in the arms and legs, but not weakness.
Pure sensory variant affects the coating of the nerve and myelin.
Miller Fisher Syndrome is mild GBS that can overlap with other variants of GBS where it restricts eye movement (Internuclear Ophthalmoplegia), causes difficulty walking or imbalance (ataxia), and loss of reflexes (typical with all variants). Miller Fisher Syndrome can evolve into a classic lack of motor sensory in the legs.
Bickerstaff brainstem encephalitis affects the brain causing confusion, altered levels of consciousness, and causes changes in the brain that are visible with a MRI procedure because it has a gq1b antibody.
Pure Motor causes only motor symptoms of the entire body.
Classic Sensorimotor results in motor and sensory syptoms affecting the entire body.
Paraparetic causes motor and sensory symptoms in the legs.
Acute Inflammatory Demyelinating Syndrome (AIDP) is the most common GBS variant with clinical symptoms of weakness or sensory changes that have symmerical weakness in both feet and up, or vice versa.
Acute Motor Axonal Neuropathy (AMAN) is rapidly progressive weakness and paralysis from its effect on primary motor nerves.
Acute Motor Axonal and Sensory Neuropathy (AMSAN) is the acute onset of distal weakness, loss of deep tendon reflexes and sensory symptoms. It differes from AMAN because it affects both motor and sensory nerves.











CIDP Variants
CIDP is one of the most misdiagnosed conditions of the peripheral nervous system. Typical CIDP looks like motor and sensory limitations for the span of 8 weeks, with events of relapses and remission. Yet symptoms will include a lack of sensibility of arms and legs symetrically (typically from imbalances proximal and distal distribution).
CIDP atypical variants affect 10-20% of patients and include:
Distal variant - 7-15% of patients who experience motor and sensory abnormalities affecting the hands and feet symmetrically. This variant can look like a random foot drop, progression beyond 8 weeks, and loss of reflexes.
Multi-focal or Lewis Sumner Syndrome - motor and sensory abnormalities can result in asymmetrical distribution of numbness and weakness, typically affecting the arms or one arm and one leg or vice versa.
Focal-Limb Onset - the rarest variant of CIDP, it affects one limb at the plexus level where nerves are coming out from the spinal cord.
Pure Motor variant - affects only motor abilities.
Pure Sensory variant - affects only sensory abilities, resulting in no weakness or tingling, and results in abnormal sensory nerve conduction data.
Multifocal Motor Neuropathy (MMN) - a multifocal presentation resulting in possible hand, arm, leg or foot weakness and paralysis; onset has an asymmetrical presentation but with progressing it can become symmetrical.






Mimics
Mimics are found when treatments are not working and symptoms progress into other medical issues.
Mimics that look like CIDP:


Anti-Myelin-Associated Glycoproteing (ANTI-MAG) can look like CIDP but does not respond well to IVIg or steroids. It can mimic distal CIDP where the hands and feet are weak at first but progresses to other areas (predominantly numbness and weakess). Mild cases with sensory changes use symptomatic treatment while more progressive treatment leads to rituximab (b-cell depleting, creating immunosuppression).
80-90% of patients with GBS or CIDP respond well to IVIg, so if there is a lack of response, doctors need to re-evaluate the diagnosis. Yet, slow progressive conditions like ANTI-MAG make it harder to detect with its pathology being different from other conditions. If titers of ANTI-MAG antibodies are less than 50%, it means that the treatment is working.
Hereditary Amyloidosis is a condition in which abnormal protein deposits (called amyloid) form in almost every tissue in the body. Symptoms can evolve to look like other conditions such as myeloma, vitamin deficiencies, or infectious sources that can be mimics of CIDP.
Vasculitis Neuropathy is an underlying rheumatoid-neurological condition resulting in systemic illness with inflammation in the blood vessels, that can restrict peripheral nervous system function.
ALS, Motor Neuron Disease, and muscle diseases can look like motor CIDP or nerve and muscle junction.
Chronic Immune Sensory Polyradiculopathy (CISP) has regular nerve conduction studies and imbalance with blocking and there is no other kind of contributing source of vitamin deficiency, hereditary or toxin, which can be a mimic of sensory CIDP.
Paranodopathy affects 10% of patients who are misdiagnosed with CIDP. It is where antibodies attack the paranode and the node at the site, which affects nerve transition, and that could result in a block to that connection. It looks like typical numbness and weakness affecting both arms and legs.
Pan-Neurofascin Condition is where people get very weak, experience sensory changes, and are almost immediately paralyzed. They typically respond to b-cell depletion such as rituximab, and takes longer to treat, especially siince it does not respond to IVIg. Rituximab is one of the first treatments for conditions tha IVIg cannot help, yet it has a 40% efficacy rate, so some people opt out of taking it. Significant nerve damage is harder to reverse.
CANOMAD Syndrome is a special case which can be a mimic of GBS or CIDP because it can affect eye movement, it changes the coding of the nerves, resulting in abnormal nerve conductions and imbalanced neuropathy.










Supporting Australians with GBS, CIDP, MMN and related conditions.
© GBS CIDP Support 2025. All rights reserved.
ABN 99 400 279 454


242 Elsworth Street West,
Mount Pleasant VIC 3350
0484 293 889
0412 180 971



GBS CIDP Support is a Registered Charity with the Australian Charities and Not-for-profits Commission (ACNC) and is endorsed as a Deductible Gift Recipient. All donations of $2 or more towards our cause are Tax Deductible.

