What is
Chronic Inflammatory Demyelinating Polyneuropathy
(CIDP)?
Chronic Inflammatory Demyelinating Polyneuropathy is a rare disorder of the peripheral nerves characterised by gradually increasing sensory loss and weakness associated with loss of reflexes. It is also sometimes called Chronic Inflammatory Demyelination Peripheral neuropathy.
CIDP is caused by damage to the covering of the nerves, called myelin. It can start at any age and is more frequent in men than women.
The number of new cases per year of CIDP is about 1-2 per 100,000 people, but as the disease can be present in a person for years prior to diagnosis, the accumulation of cases over time may be as high as 9 per 100,000 in some areas.
What causes CIDP?
The current theory is that the body’s immune system, which normally protects itself, perceives myelin as foreign and attacks it.
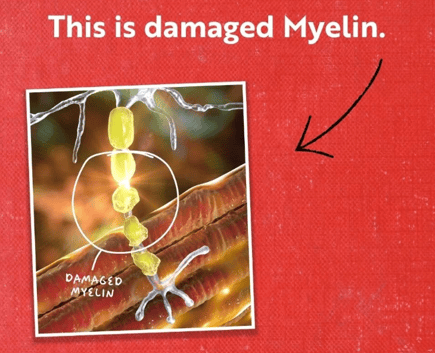
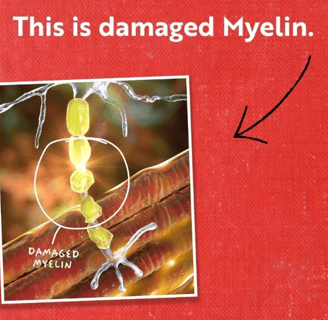
Myelin is an important part of the peripheral nervous system. It wraps around the nerve axon (the long, wire-like part of a nerve cell) much like insulation around an electrical wire. The nerves extend from the spinal cord to the rest of the body, stimulating muscle contraction and transmitting sensory information back to the nervous system from receptors in the skin and joints. This insulation (myelin) allows electrical impulses to efficiently travel along the nerve axon.
When myelin is damaged or removed, these electrical impulses are slowed or lost, and messages transmitted from the brain are disrupted and may never make it to their final destination.
What causes this process is not yet clear.
How is CIDP diagnosed?
Diagnosis of CIDP is based on the symptoms of the patient, such as loss of sensation (numbness), abnormal sensation (tingling and pain), loss of reflexes, and weakness (difficulty walking, foot drop).
Tests may include:
blood and urine tests (to rule out other disorders that may cause neuropathy and to look for unusual proteins)
nerve conduction and EMG (usually showing a demyelinating neuropathy)
spinal tap for fluid analysis (usually showing elevated protein with normal cell count)
nerve biopsy (to rule out other disorders that may cause neuropathy, usually taken from the back of the leg, just above the ankle).


How is CIDP treated?
Many people with CIDP benefit with treatment. Although there is a wide spectrum of how severely people with CIDP can be affected, some may require assistance to perform daily tasks. In the more severe cases, devices like wheelchairs or walkers may be needed for mobility. One of the goals of early diagnosis and proper treatment is to avoid this level of disability and to improve the long-term outlook.
There are three standard or first line treatments in CIDP:
Corticosteroids (Prednisone, Prednisolone) are similar to naturally occurring anti-inflammatory hormones made by the body, and can be used as an initial treatment. Corticosteroids often improve strength, are conveniently taken by mouth, and are inexpensive. Side effects however can limit long-term use.
High-dose Intravenous Immunoglobulins (IVIg) contains naturally occurring antibodies obtained from healthy volunteers. IVIg is given through a vein over the course of several hours. There are also newer treatments with preparations of higher concentrations that can be given under the skin (subcutaneous).
Plasma Exchange (PE) or Plasmapheresis (PLEX) is a process by which some of the patient’s blood (which may contain harmful antibodies) is removed and the blood cells separated. The liquid plasma portion of the patient’s blood is removed and donor plasma added before the blood is returned to the patient through a dialysis machine over several hours and repeated over several days.
There are a large number of so-called “second line” drugs used to treat CIDP. These are used when the above standard treatments fail, cause significant side-effects, or the clinical response is not optimal. These drugs are largely not tested in randomsed controlled trials, but their use is supported by case series from the medical literature.
There are a number of so-called "third line" treatments, usually chemotherapy drugs, but these should be given only in selected circumstances and by those with extensive experience in their use.
If treated early, most CIDP patients respond well to therapy, which can limit the damage to peripheral nerves and contribute to improved function and quality of life.
Living with CIDP
Post-treatment life depends on whether the disease was caught early enough to benefit from treatment options.
Patients respond in various ways. The gradual onset of CIDP can delay diagnosis by several months or even years, resulting in significant nerve damage that may limit and delay the response to therapy.
The chronic nature of CIDP requires long-term care of patients.
Accommodations in the home may be needed to facilitate daily living activities.







The Bad News
The bad news is that nerves are the slowest healing tissue in the body.
They can only heal about one inch/2.6cm per month.
This may sound like a lot, but it really is't...
Because you have 90,000 miles/144,841km of nerves in your body.
This means that it would take your nerves multiple lifetimes to heal on their own.
To view the European Academy of Neurology/Peripheral Nerve Society guideline on diagnosis and treatment of chronic inflammatory demyelinating polyradiculoneuropathy: Report of a joint Task Force—Second revision, please click here.

Supporting Australians with GBS, CIDP, MMN and related conditions.
© GBS CIDP Support 2025. All rights reserved.
ABN 99 400 279 454


242 Elsworth Street West,
Mount Pleasant VIC 3350
0484 293 889
0412 180 971



GBS CIDP Support is a Registered Charity with the Australian Charities and Not-for-profits Commission (ACNC) and is endorsed as a Deductible Gift Recipient. All donations of $2 or more towards our cause are Tax Deductible.

